fix your eyes
on what matters most
THE LEADING CAUSE OF VISION LOSS
Macular Degeneration Treatment in Melbourne & Brevard County, FL
Macular degeneration is the leading cause of vision loss and is currently an eye disease with no known cure. It causes deterioration of the retina and effects vision. It is important to begin management of macular degeneration if you are at-risk or are showing early signs of the disease.
Macular Degeneration Symptoms
If you have macular degeneration, you may see signs of the following:

Diagnosis/ Testing of Macular Degeneration
Our first-in-class technology suite provides better detection & better outcomes for your vision health.
Humphrey Field Analyzer II
Visual field testing is used to determine glaucoma severity, progression, and visual function impairment. The Humphrey Field Analyzer is an industry-recognized standard for visual field testing. It is used to detect and manage glaucoma at all stages. Various testing protocol are used for screening and monitoring early to advanced glaucoma. SITA SWAP, an additional test run using the Humphrey Field Analyzer, is used specifically to detect glaucoma in its earliest stages. This helps you get the treatment you need quickly and efficiently.
Our visual field testing completed using a Humphrey Field Analyzer is a painless diagnostic test that requires you to press a button each time a light appears on a dome. The accuracy or inaccuracy from the test helps us identify any weaknesses in your vision that may indicate glaucoma.
Why We Use the Humphrey Field Analyzer II
- Precision – This diagnostic tool is proven to provide accurate, reliable results.
- Early Detection – Identify vision loss due to glaucoma earlier than other technology.
- Speed – Complete in under two minutes.
- Accessible – Can be used by patients in wheelchairs or with visual and hearing impairments.
- Focal vs. Diffuse Vision Loss Recognition – Allows for better treatment plans.
- Comparison and Baseline Measurements for Diagnostics – Pulls data from age-matched populations to improve accuracy.
OCT Glaucoma Detection
Glaucoma is practically undetectable until the disease has destroyed the better portion of your eye’s nerves. But now, with the help of OCT Glaucoma Detection, we are able to measure the thickness of your retinal nerve fiber layer. This means earlier detection (by up to six years) and earlier treatment. OCT Glaucoma Detection is also able to identify onset of macular degeneration.
YAG Laser Capsulotomy
We also offer YAG treatment post cataract surgery, for individuals that develop a condition called posterior capsular opacification (PCO). This occurs when the back part of the lens capsule, which was left intact during cataract surgery, becomes cloudy or hazy. After the YAG laser capsulotomy, patients typically experience improved vision quickly, with little to no discomfort.

Humphrey Field Analyzer II
Visual field testing is used to determine glaucoma severity, progression, and visual function impairment. The Humphrey Field Analyzer is an industry-recognized standard for visual field testing. It is used to detect and manage glaucoma at all stages. Various testing protocol are used for screening and monitoring early to advanced glaucoma. SITA SWAP, an additional test run using the Humphrey Field Analyzer, is used specifically to detect glaucoma in its earliest stages. This helps you get the treatment you need quickly and efficiently.
Our visual field testing completed using a Humphrey Field Analyzer is a painless diagnostic test that requires you to press a button each time a light appears on a dome. The accuracy or inaccuracy from the test helps us identify any weaknesses in your vision that may indicate glaucoma.
Why We Use the Humphrey Field Analyzer II
- Precision – This diagnostic tool is proven to provide accurate, reliable results.
- Early Detection – Identify vision loss due to glaucoma earlier than other technology.
- Speed – Complete in under two minutes.
- Accessible – Can be used by patients in wheelchairs or with visual and hearing impairments.
- Focal vs. Diffuse Vision Loss Recognition – Allows for better treatment plans.
- Comparison and Baseline Measurements for Diagnostics – Pulls data from age-matched populations to improve accuracy.

OCT Glaucoma Detection
Glaucoma is practically undetectable until the disease has destroyed the better portion of your eye’s nerves. But now, with the help of OCT Glaucoma Detection, we are able to measure the thickness of your retinal nerve fiber layer. This means earlier detection (by up to six years) and earlier treatment. OCT Glaucoma Detection is also able to identify onset of macular degeneration.

YAG Laser Capsulotomy
We also offer YAG treatment post cataract surgery, for individuals that develop a condition called posterior capsular opacification (PCO). This occurs when the back part of the lens capsule, which was left intact during cataract surgery, becomes cloudy or hazy. After the YAG laser capsulotomy, patients typically experience improved vision quickly, with little to no discomfort.
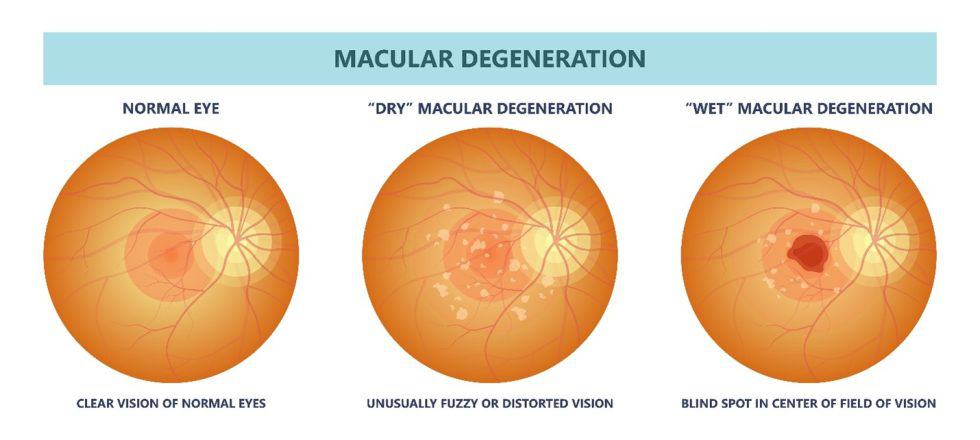
Doctors have identified two distinct types of AMD: dry and wet.
Types of Macular Degeneration
Dry AMD is the more common form of AMD. It is characterized by slower changes to the macula. Specifically, proteins accumulate underneath the macula, which can gradually impair your central vision.
Wet AMD is characterized by a much more rapid loss in vision. In these cases, abnormal blood vessels develop beneath the retina. These blood vessels leak fluids, which then distorts vision. Prompt treatment is essential with wet AMD to prevent irreversible vision loss.
Diagnosing the specific type of AMD is an important part in knowing how to best treat this condition.

MANAGING YOUR MACULAR DEGENERATION
Treatment Options
Take back control of your vision health with the most modern macular degeneration treatments available today.
Many of our patients with wet AMD can significantly slow their vision loss with injectable medication. Our doctors offer Avastin, Eyelea and Beovu. While none of these are injections are a cure, they can all block vascular endothelial growth factor (VEGF), a protein that generates new blood vessels. By preventing new faulty blood vessels, this limits leakage that can further impair vision. These injections are made directly into the eye, and typically are repeated every month to few months for maximum effectiveness. Retinal injections have been used as a common treatment approach also for both wet and dry age-related macular degeneration.
TRES VISION Group also offers EyePromise vitamins, which are specially formulated with nutritional supplements to benefit aging eyes and slow the progression of dry AMD. Specific vitamins that the American Academy of Ophthalmology recommends after a dry AMD diagnosis include zeaxanthin, lutein, vitamin C, vitamin E, zinc and copper.

FAQ
-
Who is at risk of developing macular degeneration?
There are risk factors for macular degenerations that are within the control of the individual, while others are not. Controllable risk factors include being overweight, smoking, and not using eye protection when outside. Uncontrollable risk factors of macular degeneration include age, family history, light-colored irises, and far-sightedness. It is also believed women may be more susceptible to developing macular degeneration than men.
-
How can I prevent macular degeneration from worsening?
While macular degeneration does not currently have a cure, there are actions you can take to prevent it from worsening. These include maintaining a healthy weight, eating a well-balanced diet, eliminating smoking, and exercising regularly.
-
Is there a cure for macular degeneration?
No, there is currently no known cure for macular degeneration. But there are treatment options that can be administered by your ophthalmologist.
-
What should I do if I suspect I have macular degeneration?
Please visit a doctor if you are concerned you have AMD. With a comprehensive exam, it is usually an easy condition for our doctors to diagnose. The sooner you know you have AMD, the sooner you can begin to treat it, which should help to preserve more of your vision. (Even if you do not have AMD, determining the cause of blurry or worsening vision is important.) If you notice your vision rapidly deteriorating, this may indicate wet AMD, so schedule an appointment with your doctor promptly.
-
What causes macular degeneration?
Macular degeneration develops as the age ages. While the exact cause of macular degeneration is unknown, it is likely a combination of both heredity and environmental factors.
-
Is macular degeneration hereditary?
Not all types of macular degeneration are hereditary. However, some genes have been associated with an increased risk for developing age-related macular degeneration.
-
How much does AMD treatment cost?
The price of your macular degeneration treatment(s) depends on which treatments our doctors determine are best suited to your needs. Since AMD is an eye disease, it is covered by medical insurance plans, not vision insurance. The good news is that almost every health insurance policy includes coverage for macular degeneration since treatment is essential to preserve your eyesight. TRES VISION Group can help confirm which benefits you are entitled to.
-
Do anti-VEGF injections hurt?
Prior to treatment, your doctor will use eye drops to numb your eyes to avoid causing pain. Some patients find the medicated injections used to treat wet AMD to be mildly uncomfortable and feel some added pressure in the eye for a few hours.
-
How is macular degeneration diagnosed?
Macular degeneration is diagnosed through a combination of clinical examinations and specialized tests. During a comprehensive eye exam, our eye doctors may perform a visual acuity test to see how well you read letters from a distance. Other crucial tests include:
- Amsler Grid: Detects central vision problems typical of macular degeneration.
- Optical Coherence Tomography (OCT): Provides detailed images of the retina, highlighting changes in thickness or the presence of fluids.
- Fluorescein Angiography: Uses a special dye to illuminate areas of the retina, revealing new blood vessels or retinal changes.
- Fundus Photography: Captures detailed images of the retina that helping track changes over time.
These tests help in assessing the stage of macular degeneration and guiding treatment options.
-
At what age do people typically develop macular degeneration, and what are appropriate treatment ages?
Macular degeneration primarily affects individuals over the age of 50. However, early signs can sometimes be detected in people in their 40s. There’s no age limit for treatment; it is based on the presence and severity of the disease. Treatments can vary from vitamin supplementation in early stages to more advanced therapies like injections for wet AMD as the condition progresses.
-
What are some differences between Avastin, Eylea, and Beovu for treating macular degeneration?
Avastin, Eylea, and Beovu are all injectable drugs used to treat wet AMD by inhibiting vascular endothelial growth factor (VEGF), which reduces abnormal blood vessel growth and leakage. However, they differ in composition and dosing intervals:
- Avastin (Bevacizumab) is often used off-label for AMD and requires frequent administration, usually every four to six weeks.
- Eylea (Aflibercept) is specifically designed for eye conditions, offering longer-lasting effects that may allow for less frequent injections, typically every eight weeks after initial monthly doses.
- Beovu (Brolucizumab) is the newest among them, potentially extending the injection interval to every 12 weeks after a three-monthly loading dose, offering convenient and effective results.
-
Can you explain how laser photocoagulation is used to treat macular degeneration?
Laser photocoagulation is a treatment method used primarily for certain types of wet AMD. The procedure uses a high-energy laser beam to seal off leaking blood vessels causing retinal damage. While it can help prevent further vision loss, it’s less commonly used today due to the risk of causing immediate vision reduction and the development of more advanced treatments like VEGF inhibitors. However, it may still be considered in specific cases where the leaking vessels are well-defined and away from the central macula.
-
How often should someone at risk of macular degeneration have their eyes examined?
Regular eye examinations are crucial for early detection and management of the condition. It’s recommended that:
- Adults aged 50 and older have a comprehensive eye exam every year or two.
- Those with a family history of AMD or other risk factors such as smoking or obesity may need more frequent exams, possibly yearly or as directed by their eye doctor.
- Individuals who have already been diagnosed with some form of AMD should follow the specific monitoring schedule recommended by their eye doctor, which might include more frequent visits to track any changes or progression of the disease.
