our goal is
to fix your eyesight
so that you can fix your eyes
on what matters most
Diabetic Eye Treatment in Melbourne, FL
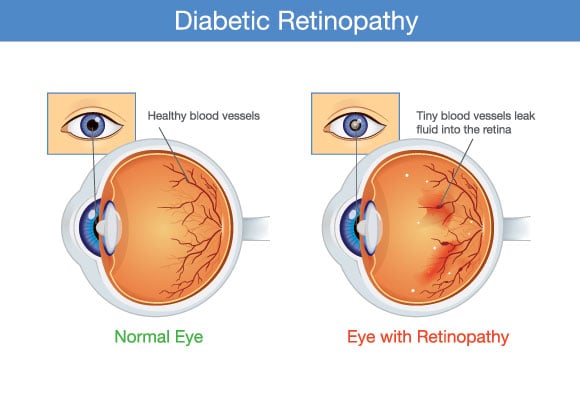
Everyone should be concerned with their ocular health, but people living with diabetes need to be extra diligent. That is because diabetic eye diseases, especially diabetic retinopathy, can cause irreversible damage — and even blindness.
Unmanaged diabetes causes blood sugar spikes, which unfortunately can damage the blood vessels in your retina. New blood vessels develop to compensate, but these are also prone to leaking, further disrupting your vision. Patients with diabetic retinopathy often go on to develop related eye problems like glaucoma, retinal detachment, and macular edema.

Symptoms of Diabetic Retinopathy
The symptoms of this disease are often difficult to discern in the preliminary stages, which underscores the need to undergo regular eye exams if you have diabetes. As diabetic retinopathy progresses, you may notice symptoms that include:
- Blurry vision
- Poor night vision
- Floaters
- Red eyes
- Eye discomfort
- Declining visual acuity
- Vacant spots in your vision
- Diminished capacity for perceiving colors
Diagnosing Diabetic Retinopathy
After dilating your pupils, your eye doctor can look at the back portion of your eyes for potentially alarming signs such as retinal scar tissue, leaked blood in the vitreous, poorly formed blood vessels, or various problems with your optic nerve.
Depending on what this initial test reveals, your eye doctor can administer additional tests. Most popular is optical coherence tomography (OCT), which provides detailed images of the retina so that your eye doctor can measure the thickness of your retina. (A swollen retina indicates that fluid has leaked into the tissue.) Another option called fluorescein angiography can identify specific vessels that are leaking blood in the retina.
If you are a person with diabetes, you should undergo regular eye examinations to check for subtle signs of diabetic retinopathy, even if you have not noticed symptoms.
Ways to Treat Diabetic Retinopathy
Early on, the best way to slow or stop the progression of diabetic retinopathy is by carefully managing your diabetes. However, when diabetic retinopathy becomes more advanced or “proliferative,” medical intervention is warranted.
Anti-VEGF Medicine
VEGF (vascular endothelial growth factor) inhibitors are injected into the clear, gel-like fluid in your eye called the vitreous. This helps to release an accumulation of fluid in the eye while simultaneously stopping extra blood vessels from forming. Lucentis, Avastin, and Eylea are the three main anti-VEGF drugs, all of which are safe. Injections are administered every few months and have been found to stabilize vision in nearly nine out of 10 patients with diabetic retinopathy.
Focal Laser Treatment
With this treatment, also called photocoagulation, your ophthalmologist uses a laser to seal leaky blood vessels so that the blood no longer seeps into the retina. A similar treatment called pan-retinal photocoagulation uses the energy from a laser to stop new leaky blood vessels from emerging.
Vitrectomy
This surgery drains the vitreous from the eye so that your ophthalmologist can remove escaped blood and scar tissue that have developed due to diabetic retinopathy. After, a synthetic fluid can be inserted to take the place of the vitreous.
Whether you need to diagnose a diabetes-related eye condition or treat an existing disease, our talented eye team can help. Please call (321) 984-3200 to schedule this critical care.
